New Jarrard Inc. Poll: Six Insights into What Healthcare Consumers Are Thinking
(4-minute read)
As the Delta variant raged hot this week and hospitals began to curtail services, we asked 1,200 US adults about their thoughts and feelings about the pandemic*. Here’s what stood out:
- Nearly three in 10 people say the current COVID-19 situation has them less likely to seek in-person care.
- Telehealth is sounding better to many, with more than four in 10 saying today’s environment makes them more likely to go that route.
- About half of those who aren’t vaccinated are dug in to their position. In fact, they’re so dug in that many of them say they’d leave their jobs rather than comply with an employer mandate.
- Sixty percent of the people who are vaccinated harbor some ill will towards those who aren’t.
Several questions continue threads we’ve been pulling in our various consumer surveys over the past 16 months. In each, we want to understand people’s feelings of safety in different settings. (See findings from last April, August and this January.)
Here’s the latest healthcare consumer intelligence:
In-person care has some people nervous. We asked consumers if the current COVID-19 situation has changed the way they’ll seek non-emergency care – in person and via telehealth. Twenty-eight percent said they’re less likely to pursue in-person care. A smaller proportion is actually more likely to seek in-person care. (Yeah, we don’t get that either. Maybe they think wait times will be shorter?) But, the largest shift is in the wrong direction – a tough situation for providers who had a taste of returning volumes this year and now may be facing the need to scale back services due to the latest surge.
Does the current COVID-19 situation affect the likelihood you’ll seek non-emergency medical care in person?
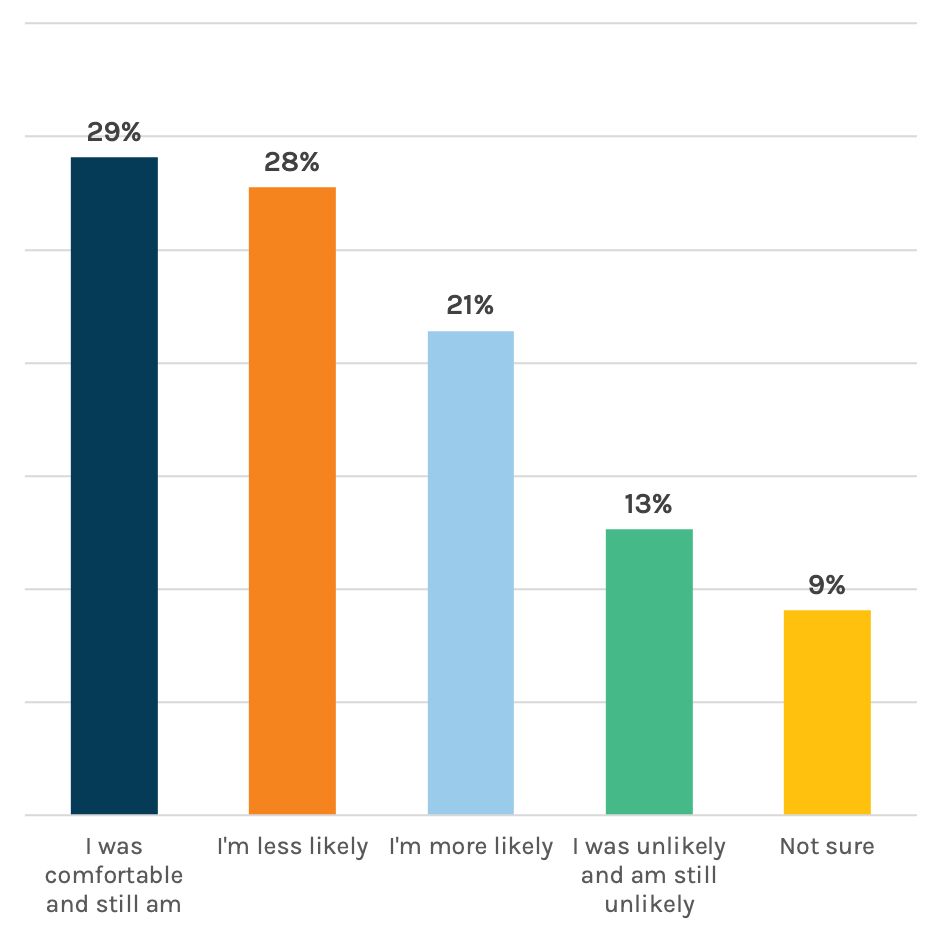
On the other hand, it looks like providers can expect an uptick in patients seeking remote appointments, as 44 percent said the current situation makes them more likely to pursue the virtual route. It’s a great reminder that telehealth needs to stay front and center. Marcom teams should play a strategic and tactical role here, helping shape public perceptions of safety, comfort, convenience and different options for care. It pays to keep patients abreast of any changes along the entire care process – from scheduling to arrival to checkout and billing.
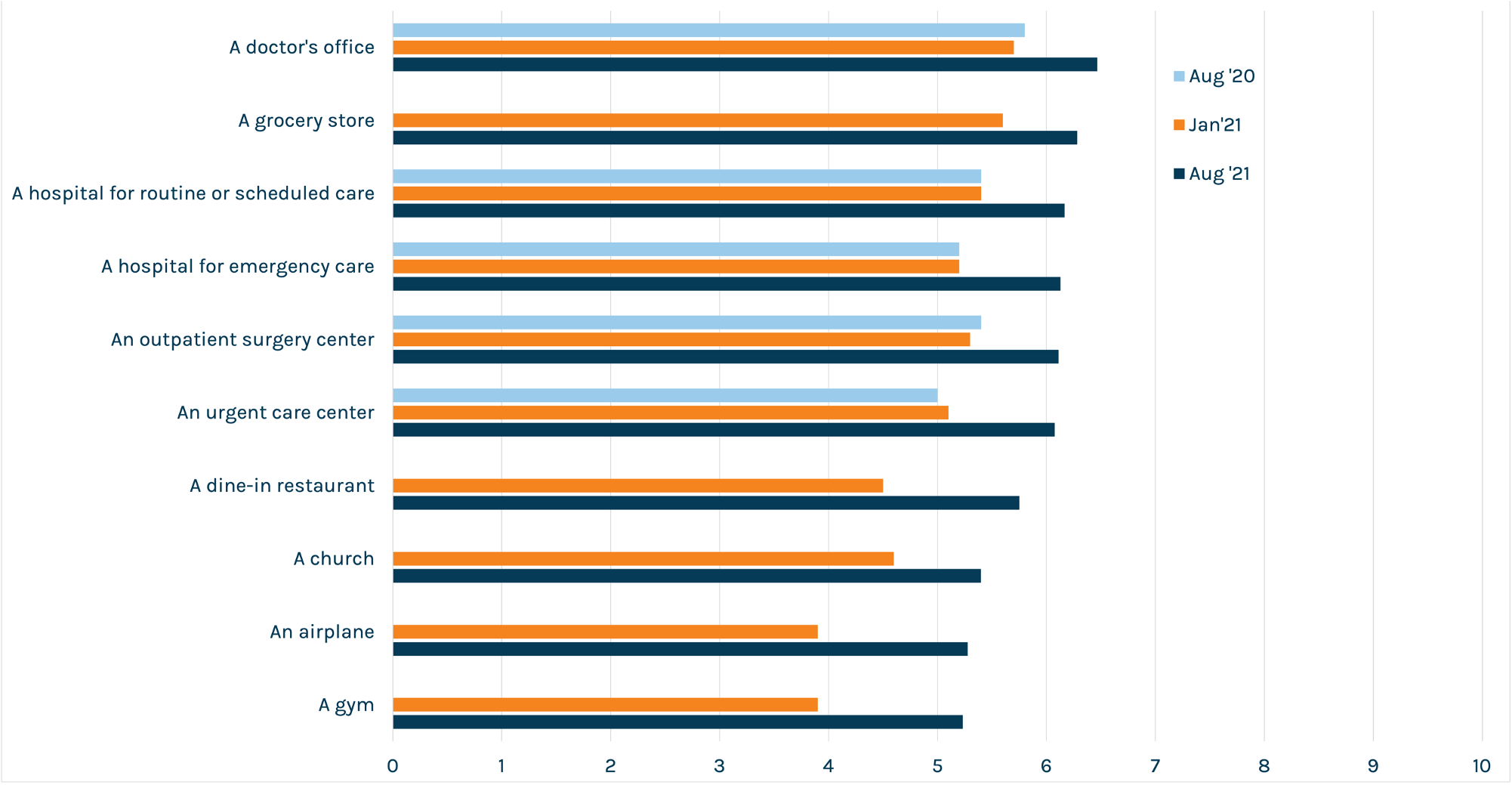
People feel a bit safer in public places now vs. January and continue to feel safer in medical settings over other locations. We’ve been asking this question for the past year. Overall, people’s feelings of safety are up roughly one point from eight months ago, based on our 10-point scale with higher meaning safer. It’s something, but not a lot to bank on.
On a scale of one to 10, how safe do you feel going into…
Vaccines and masks help allay fear. Many providers are already taking valuable safety approaches that their patients appreciate. But we wanted to dig deeper into respondents who are iffy about their feelings of safety in medical settings.
Asked what factors might help them feel better about in-person care (for non-emergencies), one of the top signals that cohort is looking for is a vaccine mandate.
We’re well-aware that many hospitals are struggling with the decision to implement mandates for employees. It’s a tough call. Still, in the public’s eye, mandates are vital to ensuring their comfort in your facility. Almost eight in 10 respondents in our January poll said that vaccinations should be required for healthcare workers – and this remains a consistent theme. So if you’ve got one in place, make sure you let the people know.
Other top factors in increasing feelings of safety were:
- Isolation of infectious diseases in separate facilities
- Masking requirements for everyone in the facility
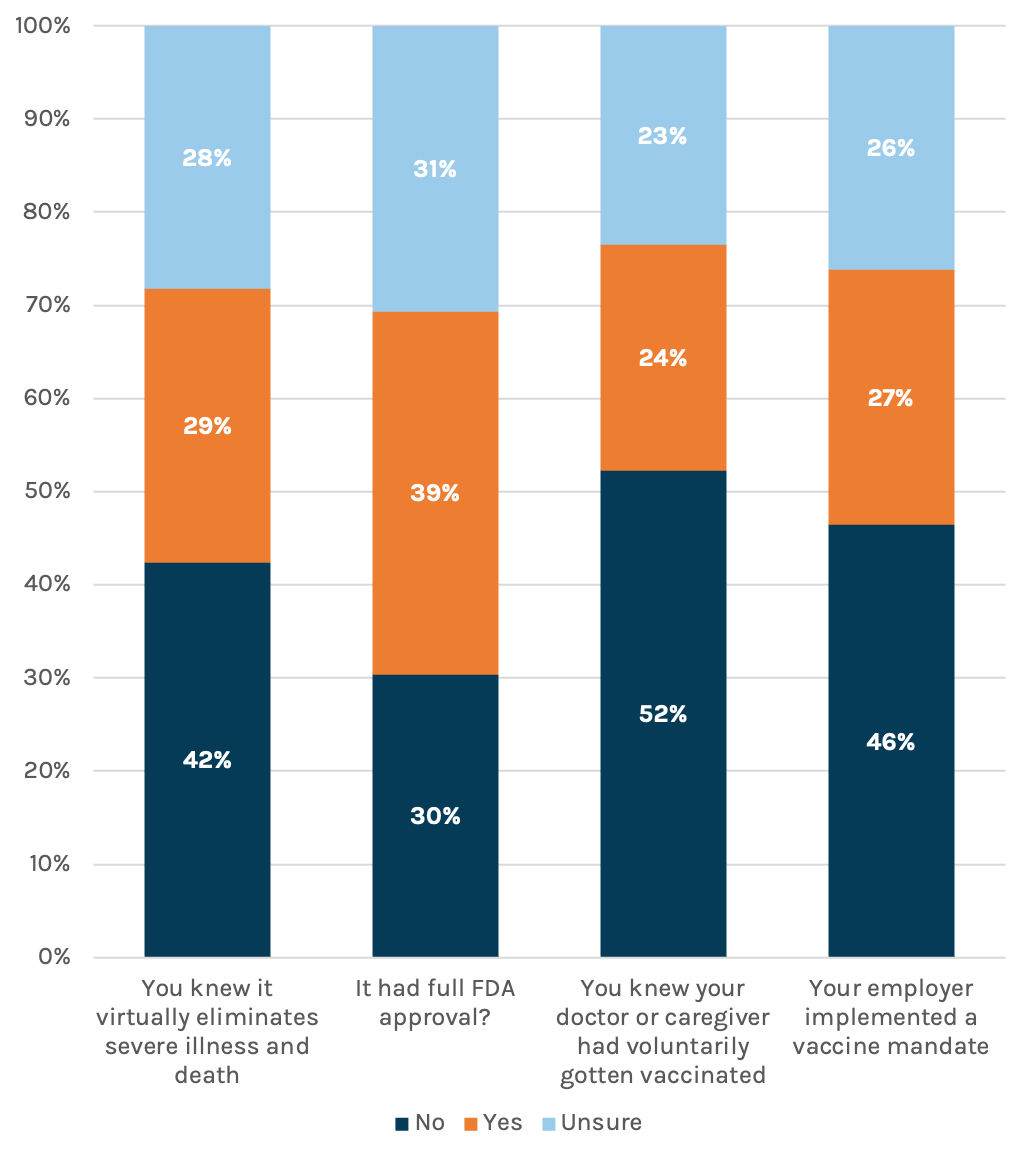
Vaccine resistance is hard-baked for a small but notable percentage of respondents. Almost 70 percent of respondents said they were either fully or partially vaccinated, perfectly in line with CDC data out this week. We asked the remaining percentage about things that might help move them towards vaccination. For about four in 10 – or 13 percent of all respondents – the answer is, pretty much nothing. In fact, we asked if an employer mandate would increase their likelihood and phrased the options as “Yes – I’d do it to keep my job,” “No – I’d leave my job,” and “unsure.” Forty-six percent of the unvaccinated said they’d leave their job rather than comply with a mandate.
For providers, that unfortunate finding is a reminder to spend time and resources where you can make change happen, because there are corners of the community where you can’t.
Would you be more willing to receive a COVID-19 vaccine if…
Those who are vaccinated aren’t thrilled with those who didn’t get the jab. No surprise, our country is divided. Sixty percent of the vaccinated said they’ve become angrier at those who aren’t since news hit of the Delta variant surge. That anger extends to the medical community, including the doctors and nurses caring for those patients who made the choice – sometimes loudly – to avoid vaccination. Each day, these professionals see the accusations and misinformation. Then they come to work to deal with the avoidable consequences of it all.
Marcom leaders need to continue keeping open lines of communication with staff, keep support resources in place and simply be aware that it’s happening.
Have reports of the Delta variant changed your opinion of those who choose not to get vaccinated?

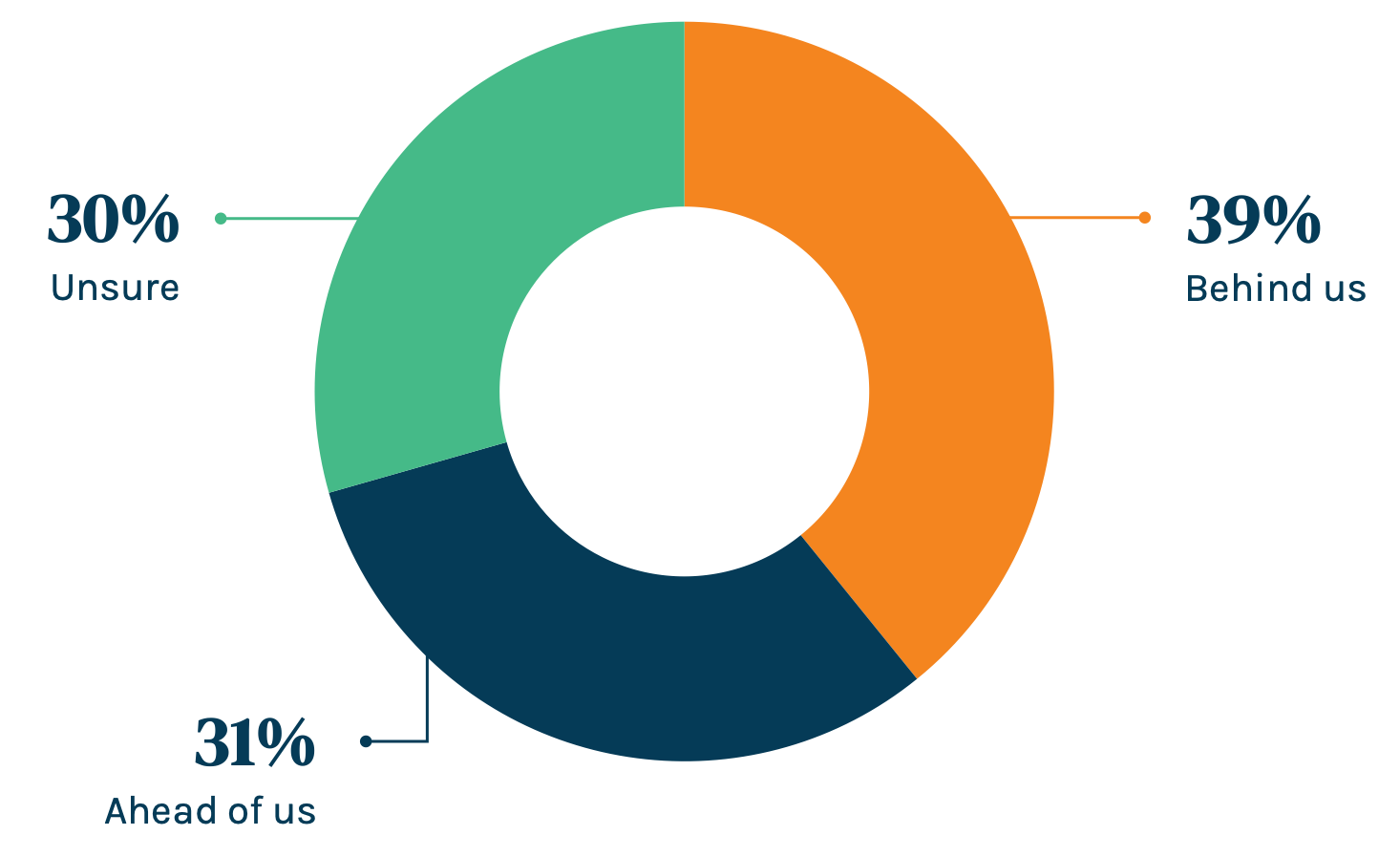
People think the worst is behind us…barely. On a brighter note, a slight plurality – 39 percent – said that they think we’re on the right side of this pandemic. Wishful thinking? TBD. Let’s hope they’re right.
Do you believe the worst of COVID-19 is behind or ahead of us?
*Online poll of US adults ages 25 and up, fielded Wednesday, August 4
Gender: 53% M / 47% F
Ethnicity: 67% white / 13% Black / 12% Latino/Hispanic / 4% Asian
This piece was originally published over the weekend in our Sunday newsletter. Fill out the form for full survey results.