David Shifrin: Let’s jump in. And Mark, tell us just about some of the high-level structural challenges that healthcare organizations are dealing with today in terms of DE&I and structural racism.
Mark Wenneker: The first answer I would give around this is that healthcare organizations, and the healthcare industry, has been aware of ethnic and racial disparities in healthcare for decades. This isn’t a new problem. In the early part of my career, I published an article demonstrating that Black patients were less likely to receive important cardiovascular procedures than white patients. That was in the 1980s. That wasn’t the first piece of research that showed that. Just last week, the Journal of the American Medical Association published an entire issue on the challenges of disparities in healthcare access for ethnic and racial minorities. So this is not a new problem. To answer your question more directly, I think there’s a greater awareness now that healthcare organizations have around the importance of addressing inequity. Most healthcare organizations have a mission to serve their communities. And if they’re not addressing the reality that there are portions of their communities that are not receiving the same kinds of care, then they’re not fulfilling their mission.
LaTonya O’Neal: When we talk about the challenges that healthcare organizations really need to overcome to move the needle on health equity, there are five things to think about. One, it takes more than just good intentions and a stated purpose.
Two, moving the needle toward health equity has to start at the top with the organization’s leadership.
Three, intentional cultural change is essential. Organizations need to expect and empower every employee to take an active role in addressing health disparities.
Four, promoting health equity needs to take place both within the healthcare organization and in the community.
And five, organizations need meaningful data to inform, measure and facilitate change.
David Shifrin: LaTonya, talk about the importance of going beyond just good intentions, right? You know I think, I hope, that everyone would agree that good intentions aren’t enough. But what does that actually mean? What qualifies as good intentions and what qualifies as the work that needs to be done?
LaTonya O’Neal: When you talk about good intentions, you can’t just take steps only because it’s the right thing to do. Just because your heart’s in the right place doesn’t mean you get credit. I think the distinction is that the actual work that has to be done should be at the foundation of the organization’s mission.
And that has to be done… the work that has to be done there is really challenging, and it’s also broad. So implementing a single, specific program to address a certain issue is great, but you can’t stop there and declare that the work is done. It’s really an ongoing, continuous process. And some of the clients I’ve worked with have struggled because they do want to do the right thing, but there’s a vast gap between wanting to do the right thing, trying to do the right thing and actually doing the right thing.
So I think having good intentions is certainly a great place to start, but you have to put the steps in place to ensure that, one, the actions are going to be meaningful; two, that they’re going to be measurable; and then three, that they’re going to be sustainable.
James Cervantes: I think too what you’re referring to, LaTonya, is really cultural change, right? So it’s not just change that happens in one department or with one program or with one person who’s leading one initiative. I think what we’re seeing, and it sounds like you are as well, is that to really move the needle on health equity and become a more diverse, inclusive organization, for many of these systems, it requires a level of cultural change that, honestly, many to this point haven’t been willing to take.
So it certainly starts at the top, but it’s also finding a way to engage every employee, every leader, to have an active role in that cultural change and that journey in becoming better—for each other and for their community.
Mark Wenneker: I would follow up what James just said. LaTonya and I recently wrote an article that was published in The Governance Institute magazine that emphasized the criticality of leadership commitment and intentionality. So, good intentions have to translate to a commitment from the top, from the board, and a set of plans that are actionable and have resources behind them. And if I’m talking to an organizational leader who’s asking me about what they do or what they should do around addressing inequities and disparities, that would be the first question: do you have your board on board and do you have a plan?
David Shifrin: Let’s talk a little bit about what you’re talking about, Mark, with the specific plans and how you build… It’s the, what is it? The SMART framework? The… Of course now I can’t think what the acronym stands for. Measurable…something: Measurable, Actionable, Timely.
What does the S… anyway… Specific! So there have to be specific goals and plans, and then also the overarching communications and mindset, and really change management that has to take place at almost a human level. And so between our organizations, I think we’ve got a lot of those bases covered in how we operate in the work that we do with clients.
But talk back and forth a little bit about how you merge those two things together, specifically as it relates to DE&I work.
LaTonya O’Neal: Change management is tremendous. It is the thing that I think, no matter the initiative in an organization, that’s required. If you don’t have a good change management process in place, you’re probably not going to be as successful as quickly in whatever that initiative is—but certainly when you’re talking about diversity, equity and inclusion, because everyone’s coming in with their own thoughts, ideas, sentiments on diversity, equity and inclusion.
You’re asking folks to align to a common idea, a common culture that speaks around the idea that you’re not going to allow inequities to occur within your organization as employees, but also that you’re going to try to resolve those inequities within direct patient care. And so I think it’s a bit of a challenge in at least some of the organizations that I’ve spoken with, it’s… even if you set up that structure, without the change management component of it, you run the risk of that idea or that initiative being abandoned because there aren’t any steps in place to make sure that you have that sustainability.
If your three highest admitters are not on board, what’s the consequence to the organization if they decide they don’t want to practice in your organization anymore. I mean, that’s an extreme example, but those are the kinds of things that I think minimize the effectiveness of some of the programs that might be out there even with well-intentioned folks, is that if these folks are not on board with it, then we must abandon it because we can’t survive without them.
James Cervantes: I think that’s a really important point; it’s having that initial buy-in, and that may take time for some organizations to build. And then beyond that, it’s really creating the awareness about what we’re doing and why, and making sure that everyone understands what our intentions are.
That we have buy-in from the board, we have buy-in from our leaders and here’s why we’re doing it. I think what makes this so challenging as well is that race and inequity is personal for many, right? We’re not talking about rolling out a new electronic medical record. We’re talking about deeply rooted issues that are very personal, very complex, very sensitive.
And so where we’ve seen some organizations struggle is just the way that we talk about it in identifying the problem. And so, one thing that we’ve done for a health system is just develop a language word bank so that we have a common definition set around how we talk about diversity, equity and inclusion across our health system and with each other so that we can all agree on something. And that, we’ve found, really built some momentum and created a more safe place for those conversations to happen.
Mark Wenneker: One area that I think healthcare organizations… after there’s been a verbal commitment made at all levels, that they really can quickly start working on is measurement. You can’t change what you haven’t measured, and healthcare organizations can readily look to see whether there’s diversity in their workforce, to have that data.
They can begin if they’re not already looking at whether there’s differences in how they treat patients. The kinds of care that they received. Their access to services. Whether there are differences by racial and ethnic background. Those are things that can be looked at. And that’s where you can start and identify those areas where there might be the greatest opportunity.
LaTonya O’Neal: You’ve got to start by defining what “it” is, right? Before you even talk about putting in measurement you’ve got to know what it is you’re measuring. And I think that that’s a challenging thing to do. And I think if you don’t start with defining what it is you’re trying to solve for, and then establishing those metrics that you’re going to measure yourself up against, it’s just a lot of busy work.
David Shifrin: One more question before we get into some of the specific examples. In thinking about both the internal and external work… so, advancing this work inside the organization and developing a more diverse workforce and getting people rallied around change in diversity equity and inclusion, and then also doing things that are going to improve patient care and the relationship between the provider organization and the community that it serves.
I hope nobody would see those as two separate initiatives. But I think it can be difficult to really know how to bring them all together. So how do you all think about that as sort of a continuum under the same umbrella?
Mark Wenneker: David, while they all really fall under the umbrella of addressing disparities in care and access, they really are separate strategic initiatives in my mind. So, the activities and focus and resources that need to address social determinants of health are very different than what needs to get done to address access to a healthcare organization. And I think both are important. So, healthcare organizations need to spend time thinking about who their community partners are and what their role is in supporting the community’s efforts to address social determinants of health.
It may be purely resources. Money. Or it may be something more direct like providing staffing or support. But it’s a very different type of work.
James Cervantes: I would agree with that. I do see them as separate, but I do think they are interrelated. Especially for healthcare organizations in more small and rural communities, where oftentimes your workforce is an extension of the community. So, how you’re talking about equity, where it sits on your strategic priority plan, how it’s mentioned in your vision and values, I think speaks volumes to your workforce.
And what you’re doing proactively, externally, I think, also needs to mirror how you talk about it and how you treat your workforce internally. So I agree a hundred percent, I think they’re separate, but there are connection points because they all sort of ladder up to the same overall vision and values.
LaTonya O’Neal: Yeah, they’re separate but not mutually exclusive.
Mark Wenneker: Yeah, I think that’s a great point, James. Most healthcare organizations are the biggest employers in the communities that they serve. So you really can’t think about that completely separately. You’re absolutely right.
David Shifrin: Well, let’s talk through some specific examples. You are doing this work, you’re researching this. So let’s just kind of go around the room and talk about some of the folks that you see doing a really good job. Some of the unique things that are happening across the healthcare industry and ways that colleagues and peers can kind of take some of those lessons about the things that we’ve talked about.
LaTonya O’Neal: We did a panel. Mark referenced the paper that we wrote some months ago where we were talking about leading while black, addressing disparities in our healthcare communities. We did a panel with some esteemed senior executives from some of the largest healthcare organizations around the country.
And three things that struck me in their talking that I think is a good blueprint for how others might want to try to get at addressing the disparities and also some of the issues around, you know, just racism in general. One individual said, “The best way to know what’s happening in your community is to get out in your community and actually see for yourself what’s going on.”
Part of that could be through board representation, but the other part about that is leveraging the people that work in your organization to help you understand what’s really happening. One example that they gave was they invited one of the nurses to join a board meeting one day, just to talk about what was going on in the community.
And it really made a difference in helping the board understand what the real problems were. The other thing that they mentioned was the measurement, which we’ve spoken about already. That is putting together performance metrics that truly you can measure yourself against in order to know whether or not you’re succeeding or not.
And the third thing that really struck me, it kind of dovetails on the first one around knowing what’s going on in your community. But we had one leader talk about how they’d started creating traveling grocery stores in areas where there were food deserts, right?
So, a lot of the issues that were going on in their particular community had a simple problem of… and I say simple not in that it’s a simple problem but as straightforward a problem of… our folks are not getting the food that they need to stay healthy and to be able to thrive.
And so, they took it upon themselves to create these traveling grocery stores so that those individuals who couldn’t get out and get the food that they needed, they provided that service to the folks within that community. Other stories like that, of being creative about how do we serve our community in the way that our community needs to be served, it’s just very important in order to make sure that we’re actually addressing the root causes of the problems that we’re experiencing.
David Shifrin: LaTonya, keep going on that a little bit, if you would. Leadership recognizes the need to go out and understand what’s happening and what needs to be done. They make the commitment to go out. They go out—whether to the community or inside the organization.
What does it look like practically for a leader to step into that conversation and listen and extract the information that they can then take back and use?
LaTonya O’Neal: You know, it’s a great question. I know that at least with a couple of folks that we spoke with, they talked about how being a trusted leader in the community was one of the ways that they were able to actually even get people to share with them the needs that they were experiencing. And so, I think part of it is being present, being available, and not just coming in to be a speaking head, if you will, is the first way you do that.
And I think that listening to the teams that you have in your organization could be another way of doing that. It’s one thing to think that you’re going to be able to walk around the neighborhoods and knock door to door and have people to just share with you what’s going on. You’ve got to be creative in how you get that information, whether it be surveys, whether it be information you’re collecting when the patient is admitted into your service.
No panels… you’re really getting that real-world feedback. I guess the key point is not to assume that you know what the problem is.
Mark Wenneker: You know, it’s striking to me that a very close corollary of this importance of listening is, who is actually representing your organization to listen? And while I think we need all leaders, regardless of their background to be present—as LaTonya is saying—in the community, it is very important that organizations have leaders that reflect the backgrounds of their representative communities. And that’s not happening enough. Because I think the communities, when they see those leaders that have similar backgrounds, are going to feel more engaged. They’ll have more trust. And I also think the other piece of this around workforce diversity is if you have those opinions and experience brought into your organization, it’s important to also listen to your community and go out.
But having that representative thinking and experience within also helps you understand what needs to be done.
LaTonya O’Neal: And too, Mark, creating that safe space which we’ve talked a lot about in the past, you’ve got to create that safe space where your teams are comfortable enough to even bring those types of ideas forward.
James Cervantes: Along those lines of listening, one thing we did at Jarrard to help facilitate conversations like that—and this was for a large health system out West—is they knew that they wanted to leverage their clinicians and physicians who for the most part their workforce and even members of their communities trusted.
But some of the folks just weren’t sure how to have those conversations, what questions to be asking, how to dispel some of the myths. They have the clinical information, but it’s how you frame it. And so we created a couple of toolkits. One was really for internal ambassadors and clinicians to use within the organization, as they’re in meetings to just address some of the top topics head on and to dispel some of those myths. But more importantly, to your point, Mark and LaTonya, to just be available to answer questions. And to really hear what the concern is from some of these groups that were very reluctant to get the vaccine. And then the other toolkit was really more for community partners. So, how were they able to leverage their community partners to engage in thoughtful conversations outside of the walls of the medical center?
And I think from both of those efforts, sort of in parallel, they saw tremendous uptick in the number of folks that were coming to get the vaccine. And I think they just have a deeper sense of who their community is now in a way that a data point wasn’t able to provide before those conversations.
LaTonya O’Neal: Just to add onto that, we created a maturity model as part of the work that we did earlier in the year as a way to help hospitals take a hard look at themselves. To look in the mirror and say, “Where are we along this continuum of where we want to be to address these disparities and make sure that we are really serving our communities holistically?”
And there are lots of other tools out there that we’ve seen. Actually, through the work that we did with the National Association of Health Services Executives, they’ve got other resources as well. But, I think that’s really important. You’ve got to take a look in the mirror and understand where you are, ask yourself those questions, and be honest about where you really are. And then put a program in place to drive toward where it is you’re really trying to head. I think without that, it again is well-intentioned, but it’s certainly not going to move the needle in a way that’s going to be measurable and impactful.
David Shifrin: Okay. LaTonya, Mark, James, what did we miss? What do you want to chat about?
Mark Wenneker: You know, there’s… the only other thing I was thinking about in terms of topics, was this issue around, is there a business case to be made?
So, in our report, that we did in collaboration with NAHSE, we talked about one of the challenges that healthcare organizations are facing, which is the question about, “How do we invest in these important areas, given the challenges we’re facing financially—most acutely with the pandemic, but certainly in the long term?” And yes, those are real. Those are real issues. However, it’s important to understand that the societal impact of healthcare disparities from a financial standpoint is significant. A Kaiser Family Foundation report estimated that disparities contribute almost $100 billion dollars in excess medical costs to our society and $42 billion in lost productivity.
Now that’s not to say that healthcare organizations can always capture those savings by making investments, but I think it’s important that they in their planning think through how can they benefit financially in addition to morally, their moral commitments, as they proceed with this planning work.
LaTonya O’Neal: You know, Mark, that’s a great point demonstrating the return on the investment. So, even in our consulting work, there are a lot of things that are the right thing to do that are good for the organization but might not have a return on investment. When you think about health disparities, the readmission rates that happen with patients who are not able to care for themselves at home, or when you think about extra admissions just because patients are not able to make their regular physician visits and things like that.
I mean, there is not enough data yet. I think that this is again back to where we need to really create some good measurement vehicles. But the return on the investment of making these programs part of your organization’s internal fabric and culture is significant. And in my mind, at least in working in the revenue cycle space like I do, you think about admissions, hospital care and then the billing that happens on the back end. I’m sure that there could be a direct correlation between these programs and patients do in your organizations on a regular basis.
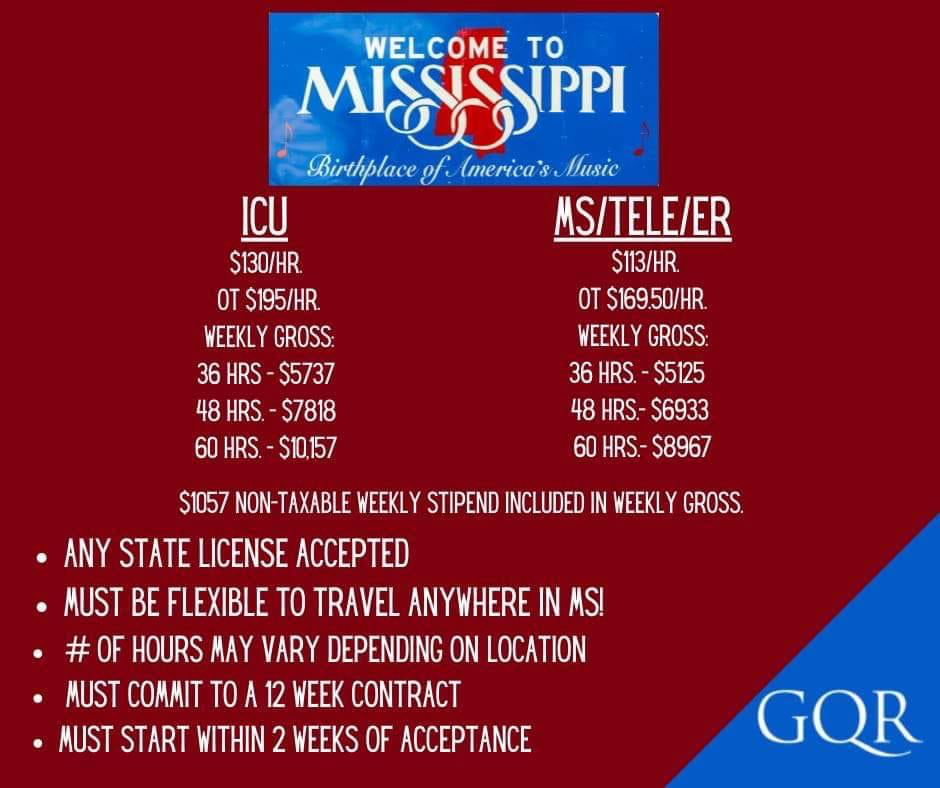
James Cervantes: I would add, too, going back to our point earlier about your workforce, the labor market is as tight as it ever has been. And so, how are you honoring your commitment to health equity and retaining the talent and bringing in top talent? And I think more people, especially younger generations, are driven by and inspired by organizations that do what they’re going to say that they do and fulfill those commitments to their community and to solving for health equity. So, I think there’s sort of the workforce element as well, from a business imperative.