High levels of public trust in healthcare workers and hospitals only goes so far in insulating provider organizations from mixed feelings about how hospitals prioritize between money and patients, how they handle access and equity and how they support their staff, according to a new survey produced by healthcare strategic communications firm Jarrard Phillips Cate & Hancock, Inc. and Public Opinion Strategies.
Two years into the pandemic, hospitals retain a high level of trust when it comes to providing critical healthcare information, and a majority of adults have a positive perception of the quality of care available in the US. However, barely half feel strongly that their preferred hospital fulfills its mission or provides equitable care, with even fewer feeling strongly that their hospital is a good community partner.
These findings highlight an opportunity and need for hospitals to build on their strengths to improve public perception and understanding regarding how thoughtful business practices allow them to meet their mission.
“Dark Suits & White Coats: Healthcare’s Acute Divide” is Jarrard Inc.’s fourth national healthcare consumer pulse check since the pandemic began. Fielded in December, the response pool included 800 adults and 200 who work in healthcare.
Key themes that emerged involve the business of care, trust and burnout.
The Business of Care
Though 62 percent of respondents think the quality of care in the US is good and meets their needs, only 50 percent strongly feel that their preferred hospital fulfills its mission. Many respondents are ambivalent or unsure about these issues, which provides an opportunity for hospitals to increase support for their approach to the business of care.
“We know hospitals and other provider organizations are doing incredible work to serve patients while operating in an extremely challenging environment,” said David Jarrard, CEO of Jarrard Inc. “In light of that, hospitals would benefit from an even greater public focus on mission to underscore their commitment to patients over finances. They can’t assume that because people prefer to receive care at a specific hospital or are happy with the quality of care that they feel good about the organization and its business practices.”
Jarrard said such soft support in the survey renders patients – and employees – vulnerable to being swayed by critics and competitors. It puts hospitals at risk of lower loyalty and open to reputational damage.
“Hospitals must go beyond looking at metrics of volume and patient loyalty and develop ways to connect even more deeply with the public in fulfillment of their mission,” he said.
Related Data Points:
- Only 41 percent strongly feel that their preferred hospital is a good community partner.
- Only 35 percent strongly feel that their preferred hospital handles patient-related financial issues well.
- Only 42 percent of consumers and 38 percent of healthcare workers, feel strongly that their preferred hospital focuses more on its patients than on its business.
Trust
Trust in doctors and nurses remains high at around 85 percent, according to the survey. And though consumer trust in hospitals did drop six points in the past year to 76 percent, they join nurses and doctors as the most trusted sources when it comes to critical healthcare information.
“Provider organizations can use that public trust to speak to and combat some of the skepticism about the business of healthcare,” said Jarrard. “That means being open about how they operate, what they’re doing to contribute to their community and how they’re delivering on their mission of care. And when missteps are made, hospitals must own them and make clear, meaningful change that people can see.”
Jarrard said organizations should also engage with nurses and doctors to speak on behalf of their organization. But before doing so, healthcare leaders must ensure that they are truly supporting and engaging team members, who are exhausted after two years of pandemic work and somewhat skeptical of hospitals.
Related Data Points:
- Consumers trust hospitals more than health officials (64 percent) and the CDC (60 percent).
- Nine in 10 consumers trust their preferred hospital, compared with 74 percent who trust health systems in general.
- Trust in hospitals has declined more among Republican voters (31 percent) than Democratic voters (17 percent).
Burnout
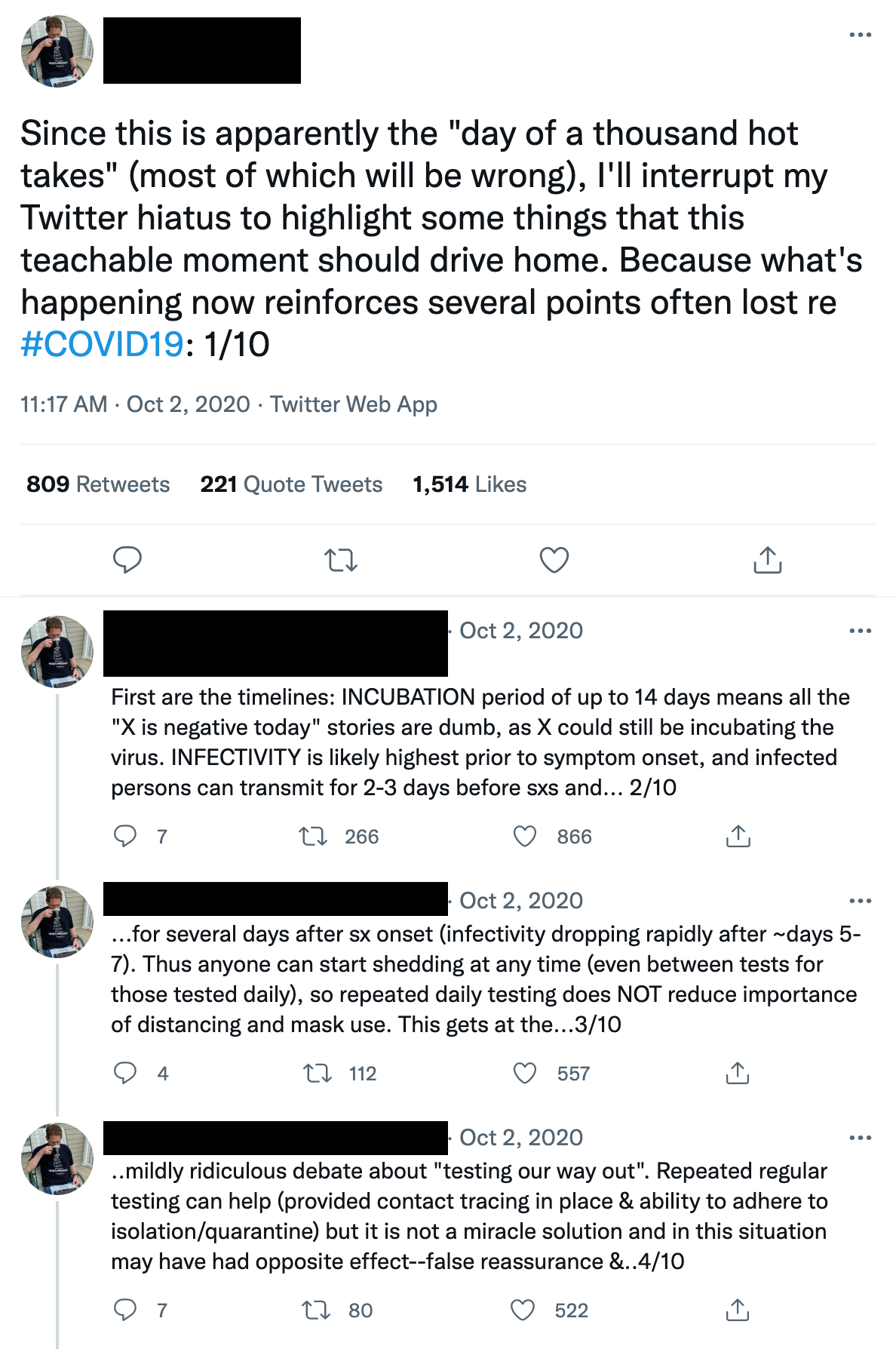
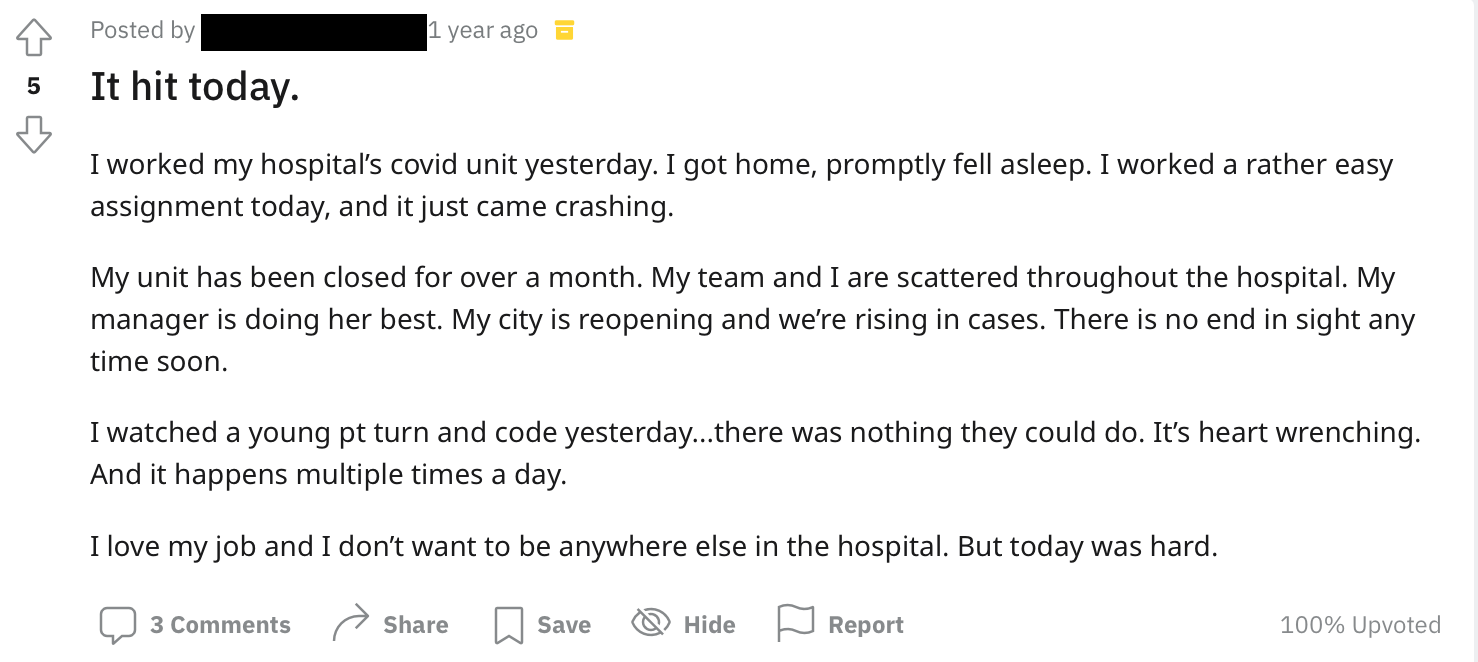
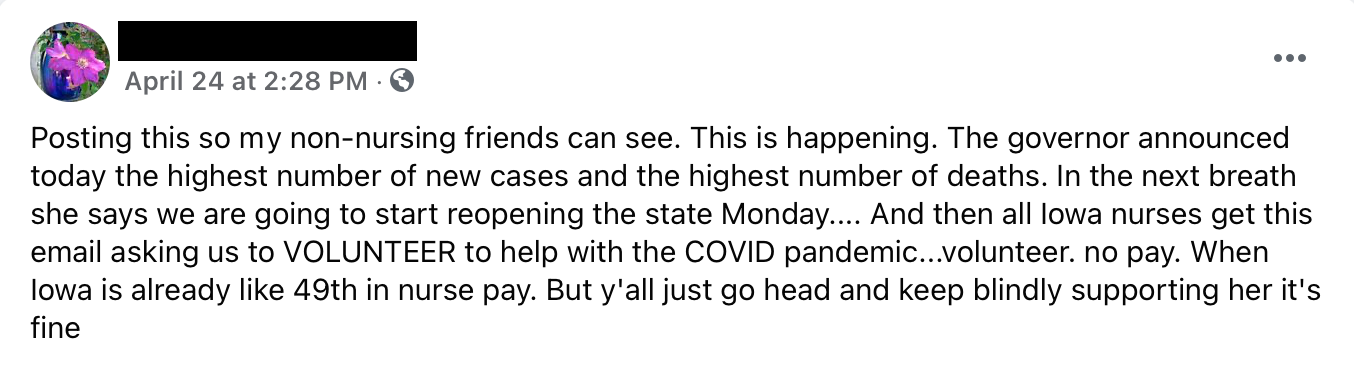
The study found more than half of healthcare workers are experiencing significant burnout. Nearly a third feel disconnected from their employer, and more than one in 10 are unlikely to remain in healthcare.
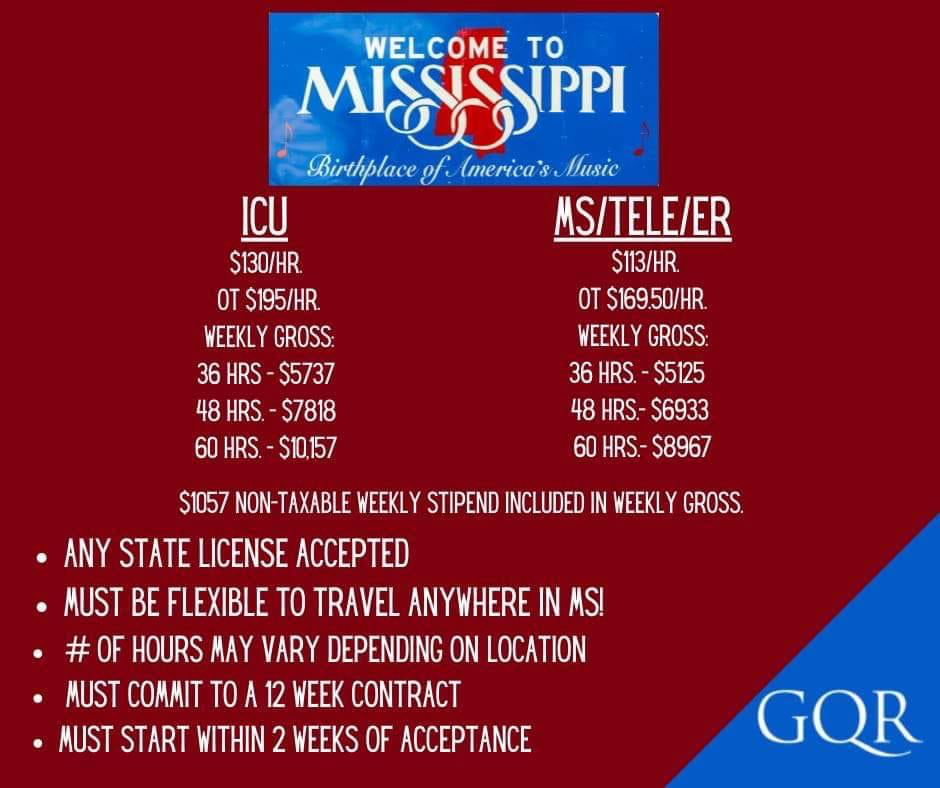
“Hospital leadership across the country has recognized the strain on the workforce and has gone to great lengths to help,” Jarrard observed. “They’re looking at compensation models, technology to streamline operations or free up resources and they’re seeking to improve recruitment and more to mitigate the challenge.”
He added that the healthcare industry may be headed toward a realignment of staff and clinicians, particularly nurses, moving away from acute care.
“In particular, if healthcare workers don’t feel connected to their employer, don’t think their employer values their mental health or have concerns that their hospital prioritizes money over patients – the bond that links them has been significantly weakened,” Jarrard said.
Related Data Points:
- 52 percent of healthcare workers are experiencing significant burnout
- More nurses (55 percent) are experiencing burnout than doctors (43 percent.)
- Some 30 percent of healthcare workers feel their employer doesn’t value their mental health.
- While 52 percent of survey respondents work in a hospital/clinic within a health system, only 32 percent said that is their ideal work environment. By contrast, only 2 percent of respondents work for travel nursing companies and health tech companies, but 6 percent and 11 percent respectively, said those options would be their ideal.
About Jarrard Inc.
With offices in Nashville, Tenn. and Chicago, Jarrard Phillips Cate & Hancock, Inc. is a U.S. Top 10 strategic communications consulting firm for the nation’s leading healthcare providers experiencing significant change, challenge or opportunity. Founded in 2006, the firm has worked with more than 600 clients in over 45 states and served as a communications advisor on more than $60 billion in announced M&A and partnership transaction communications. The firm specializes in M&A, change management, issue navigation and strategic positioning. Jarrard Inc. is a division of The Chartis Group, one of the nation’s leading healthcare advisory and analytics firms. For more information, visit jarrardinc.com.