Welcome to DigitaLee: The home of digital and social media for healthcare.
We’ve partnered with Lee Aase, formerly of the Mayo Clinic and Mayo Clinic Social Media Network. He’s joining us every other week to look at the role of digital and social media in healthcare. Each week we’ll look at a news story related to healthcare social media, a digital platform healthcare providers should (or shouldn’t) consider, and a digital tip of the week.
Today we’re covering a story about the use of social media for finding health information, an overview of the audio platform Clubhouse, and considerations for how hospitals, health systems, doctor’s offices and health services companies can build a good social media policy.
Listen and subscribe to the podcast or read the transcript below.
Read the Transcript
David Shifrin: This is DigitaLee from Jarrard, Phillips, Cate & Hancock. I’m David Shifrin. This is our first real episode. So, if you stumbled in here and are wondering what it’s about, please check out the intro, episode zero, on whatever platform you’re listening on now. In short, we’ve got Lee Aase, a pioneer in digital and social media for healthcare who just retired from more than two decades at the Mayo Clinic, among other positions. Every other week, Lee and I will review three things: a trend or headline related to digital healthcare, a social media platform, and then a quick tip for healthcare Marcom and digital teams. Today, we’re covering a story about the use of social media for finding health information, an overview of the audio platform, Clubhouse, and considerations for building a good social media policy.
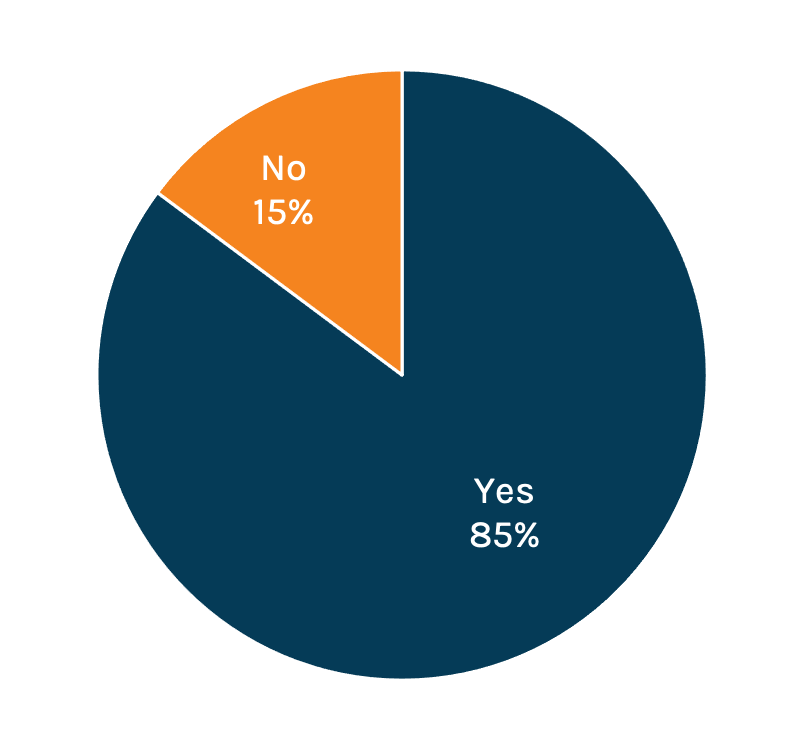
All right. So let’s kick this thing off with our first news story, an article from Forbes saying that one in ten Americans turn to social media for health information. I’m going to bias the conversation a little bit before I kick it over to you, Lee, by saying that I was really surprised that the number was only one in ten, only about 10%. I would have guessed, I don’t know, 40% maybe? But what’s your reaction to the rise of social media as a health information platform?
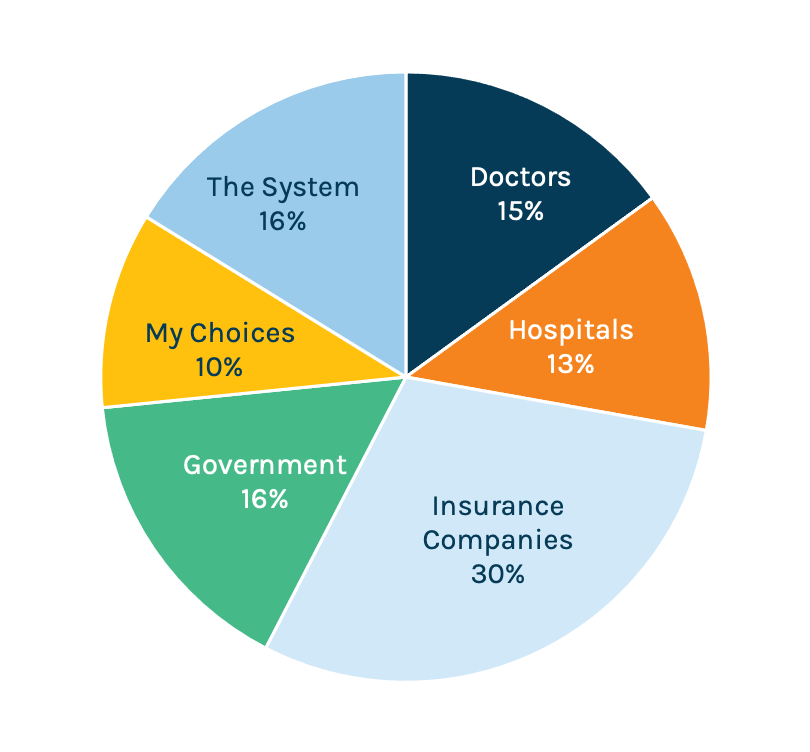
Lee Aase: Yeah, well, I think you need to put it in context that in the survey of a thousand patients like me, they found only 16% went to traditional news.
So, if you’re only at 16% for traditional news, the fact that you’re at 11% for social media isn’t that far behind. They did see that Google and disease and condition sites like WebMD and Mayoclinic.org, were kind of in that 30%-ish range, 30, 35%.
So, I think the reality is that people don’t go to social media, they go to their friends. It isn’t like social media in general, but they’re looking at what did the people that they connect with on social media have to say? So I think that’s the question: Who do they really trust?
And I think we’ve seen a declining trust in some of the various news outlets that has probably brought that down. I probably would have been predisposed to think it would, that number would be for social media going in, but I think what we’ve kind of just generally seen in society is kind of a breakdown in who your trusted source is.
DS: The participation versus trust gets to another finding in there, where they found only 2% of people actually trust social media. Nine or eleven, depending on which number you’re looking at, go to social media for information, but only 2% trust it. So, that implies that it’s exploratory.
All right. Let’s turn our attention to the platform of the week or whatever we want to call this thing. There’s a new-ish, I guess it’s really not that new at this point, but still, a relatively obscure platform called Clubhouse, which is essentially live audio rooms. And I think it’s become more popular among business types over the last year or so, it’s a different way for folks to engage.
But because we are starting to see more folks bring up the idea of this interactive audio approach rather than either live chats or text-based social media. Should healthcare providers be paying attention to Clubhouse? And if so, why?
LA: Yeah, Clubhouse is a really neat platform. Twitter Spaces is an analogous platform within the Twitter universe. The whole idea behind it is it’s live interactive audio chats that instead of just listening to a recording (for the most part), you’re able to interact directly with people. Compared to regular, old-fashioned Twitter chats where people are texting, where anybody can run into the conversation, they’re much more moderated and orderly. I think there’s been a lot of growth. I think Clubhouse had a good strategy when they made the platform invitation-only at first to give it a more consistent user experience and make it feel somewhat exclusive.
That way, people had to get an invitation to be able to join, and so they perhaps valued it more.
DS: So, my first Gmail address.
LA: Like that! Or, The Facebook back in the day, you know? Because it was somewhat exclusive, it was kind of a cool thing to get an invitation, to be able to participate in it.
I have found for a lot of the same reasons that people use podcasts, and where there’s been this resurgence in podcasts as led by Joe Rogan and then so many others after that, where the fact that you can multi-task by listening and driving is a great advantage. Also, you can listen to a podcast on something of very personal interest and go into it in great depth. Likewise, some of these Clubhouse chats can go on for half an hour, forty-five minutes, maybe even an hour where you’re having a conversation and it’s moderated by leaders who are inviting people in to share their perspective.
So, it isn’t as noisy. It’s got audio, but it’s not as noisy as a Twitter chat where anybody can use the hashtag and jump in with a point.
DS: Should providers be considering using this for, a weekly health chat and getting their physicians out in the world? Or is there relevance for Marcom teams?
LA: I think there’s something to be explored there to at least test it, to see how it works in your particular context. One of the beauties of it is that, unlike Zoom, Facebook Live, or some of the other platforms that include video, there just isn’t as much production.
It can be much more informal. You can just do it with a smartphone because that’s the only way you can do it. You don’t have to be worried about hair and makeup and lighting; you can be focusing much more on the nature of the content of the conversation without having to worry about some of the aesthetics. It’s kind of like video killed the radio star, you know, back in the day.
This is sort of like the radio stars’ revenge.
DS: All right, let’s move on to the final section. We’ll get better titles for each of these sections. Tip of the day. With so much happening around nurses and doctors getting more involved in talking about their field, work, and what they’re seeing within the four walls of their facility, there is much more noise and, frankly, anger on social media, on all sides.
Consequently, it’s a really good time to be evaluating your social media policy.
What are one or two key tips for a good, strong social media policy for a healthcare provider when they’re looking to ensure that their employees are staying in line without stifling the conversation?
LA: I definitely agree with wanting to facilitate it and make it encouraging, and putting up guardrails instead of roadblocks. I think the other one of the other elements is just to make sure that you’re legal with it. A lot of times people will want to put in a policy that says, you can’t say anything bad about our organization online that reflects poorly on us. The National Labor Relations Board has said that concerted efforts and discussions around wages, hours, and working conditions are protected speech and you need to guard people’s ability to do that. So, you have to realize that there will be the good with the bad, but that you can have standards for professionalism and for mutual respect.
That rule applies whether people are on duty or off. I think the other part of it is effective communication of the policy, and that the idea isn’t to be a “Gotcha!” thing. It isn’t, “Oh, good, we can fire you.” It’s, “How do we keep people out of the ditch. How do we keep people from doing things that will reflect poorly on the organization?”
It just isn’t good practice – they get into a heated discussion and they kind of spout off on something. It’s important just to be in front of people, to be giving them guidance with examples of the kinds of things that they can do and should do, then the things that they would be best to avoid. Training and education, I think, are the really key elements.
DS: Alright, well, thanks. First episode, first conversation, in the books.
LA: Magically edited to sound super smart!
DS: You know, that’s what I do.
Subscribe to Jarrard Insights & News
"*" indicates required fields