Note: This piece was originally published over the weekend in our Sunday newsletter. Want content like this delivered to your inbox before it hits our blog? Subscribe here.
The Big Story: Biden executive order calls for action on hospital consolidation, price transparency
The President issued an executive order on Friday “telling the Federal Trade Commission to prioritize hospital consolidation in its enforcement efforts. The order will ‘underscore that hospital mergers can be harmful to patients and encourages the Justice Department and FTC to review and revise their merger guidelines to ensure patients are not harmed.’” The AHA and FAH weighed in with overviews and critiques shortly after.
Our Take
(2-minute read)
It’s a Catch-22: Scrutiny of hospital consolidation is increasing in direct proportion to the need for hospitals to find strong partners.
Biden’s executive order follows a cascade of criticism and Senate hearings directed at hospital consolidation – with one outlet going a step or three further and referring to it as “cartelization.”
Yes, the scale of deals is on the rise. A Kaufman Hall study found that the number of deals through Q2 of 2021 is down markedly from previous years, but the size of those deals is “the second highest in recent years.” And yes, some research shows such mergers can drive up prices.
What’s missing from the conversation is that consolidation is happening because the system is broken. It’s broken in myriad ways (seriously, it takes two presidents to let us buy hearing aids without a prescription!?), and we’re stuck until we create something new together.
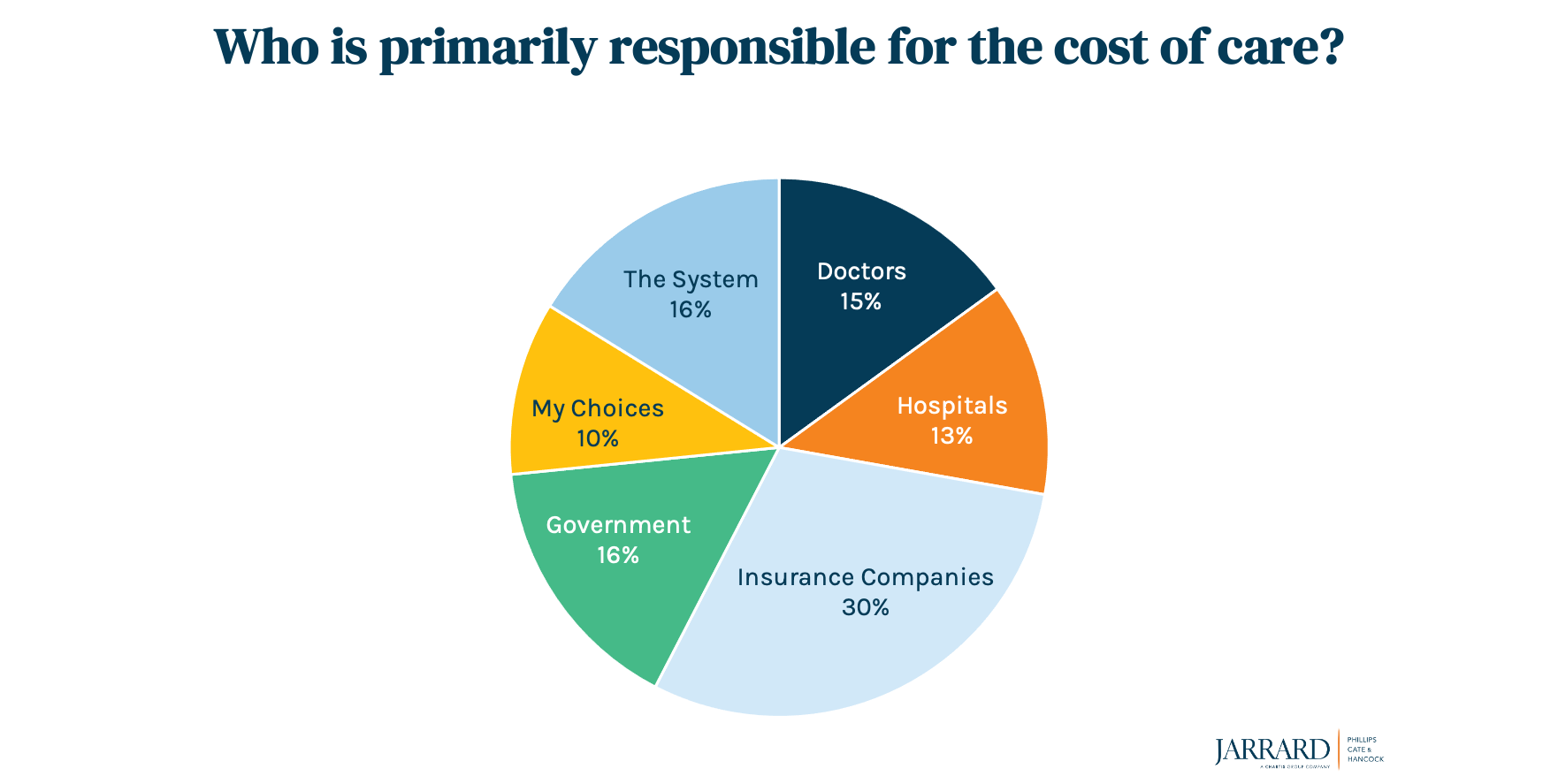
The current version of the escalating-costs narrative critics are using pins the blame squarely on providers by suggesting – implicitly and sometimes explicitly – that mergers are driven by greed. The White House fact sheet laying the foundation for the order says that “Hospital consolidation has left many areas, especially rural communities, without good options for convenient and affordable healthcare service.”
It’s a compelling narrative. Our question: Where’s the counter? Who’s telling the story of the real reasons a hospital might want – that is, need – to join a larger system? Or of what might happen if they don’t partner up? There’s a taste of that in the AHA and FAH statements, but more is necessary.
It’s time for hospitals and those who care deeply about access to healthcare to build that narrative. To speak up.
Hospitals can and do pursue mergers, acquisitions and partnerships for a variety of reasons. First among them is so they can continue to fulfill their missions. Over and over, we’ve seen hospitals stay open because of a deal.
Which brings up a related reason for deals. Rural providers often have no other option because the math isn’t working in their favor. The government pays as little as 50 cents on the dollar through Medicare and Medicaid. Plus, there’s a downward push by payers to reimburse at lower rates. That means standalone hospitals – particularly smaller community hospitals where relatively little revenue comes from private reimbursement – often must choose between closing or becoming part of a larger system.
Again, you can’t care for your community if you don’t exist.
So instead of the chatter depicting health systems as predatory, let’s share the stories of community providers seeking a partner for true shelter. To be able to survive. Providers and advocates for access can start engaging in that conversation this way:
- Articulate the actual value to consumers of a consolidation or merger. To be clear, this isn’t offering the same tired and vague messaging about “value,” “transformation” and “scale.” It’s a direct, honest story about what will happen if the deal goes forward…and the consequences if it doesn’t.
- Prepare for state attorneys general, health insurance companies and others to use the administration’s activity to ramp up opposition to consolidation (which challenges their market share). In other words, your government relations work and relationships with opinion leaders matter more than ever.
- Explain how you will deliver on promises made. And then do it.
This executive order appears to be a request for more action, not the action itself. That suggests there will be a waiting period, possibly even a comment period. Don’t let that time go to waste. The conversation has been underway for a while, and it’s being dominated by non-providers. Some are well-intentioned and want to improve the value and delivery of care. Others are market competitors (the self-proclaimed disruptors) and adversaries who view this as a zero-sum game and are campaigning to make providers the fall guy. Hospitals, health systems and others who are focused on access need to stand up. This is a new type of scrutiny. It’s time to respond in new ways.
How to do that? Coming soon.