Ten years ago, Gary Keller and Jay Papasan wrote The ONE Thing: The Surprisingly Simple Truth About Extraordinary Results. It quickly became a bestseller in the productivity and self-improvement genres, giving readers ways to become more productive and successful by “focusing their energy on one thing at a time.”
The book includes what the authors call “the Focusing Question,” which reads, “What’s the one thing I can do such that by doing it everything else will be easier or unnecessary?”
In the complex, endlessly noisy work you will begin (again) as another year fast approaches, what is your “one thing?”
Every December, we gather a group of healthcare insiders to talk about what they observed in the year just gone and what they expect in the months ahead. This time, our panel consisted of Jarrard Inc’s own five practice leads, each focused on a different type of healthcare provider organization.
No surprise, there were some common themes that emerged. Those are below, and most deal with an element of healthcare itself, like nurse and physician engagement, or scrutiny of hospitals.
But throughout these conversations it was striking to hear several answer the question with a question of their own. We asked “If you’re in a room with a client or executive team, what’s the question you ask to help them get unstuck?”
Their common question? “What’s the One Thing we need our people to know, to say or to do?”
As Emily Shirden, Jarrard VP and National Practice lead put it, “If we can take whatever issue it is and boil it down to a sentence or two, that helps focus on what’s most important and then figure out next steps,”
And so, with the swirl of work to be done to advance each healthcare organization in the new year, highlight The One Thing made sense as the, well one thing to highlight. Whatever else comes, pause, boil it down, and focus that moment’s energy on the single next step.
Other angles to that that question our team suggested healthcare leaders ask:
There are, no doubt, many questions to ponder as you prepare for 2024. The challenges are great, the answers are hard, and the issues many and relentless. Review themes that our team is watching, and read excerpts from conversations with each practice leader below.
Then, take a breath, if you can, and reflect on the single focusing question that helps draw the many matters before you into contrasting relief. Take the iconic advice cowboy Curly gave to a greenhorn in “City Slickers” and figure out your one thing for the new year.
How does a given organization best serve its patient population through partnerships, technology and care models? Once that question is answered, when change is coming, it’s vital to think through and talk about the implications. It’s not simply telling people what you want them to hear. It’s being a good community partner – and employer – by giving stakeholders all the information so they can make their own decisions and then listening to their thoughts through surveys, listening sessions and one-on-one conversations.
Additionally, there’s an opportunity to grow through an emphasis on aligning the external brand with the internal culture. This helps create a unified, trusted experience that patients feel comfortable interacting with.
Stronger relationships are being forged between systems, hospitals and community health providers, underpinned by a shared, community-centric mission. Tim Stewart, Partner and Academic System lead, noted the importance of using partnerships to “find the best path forward that utilizes academic innovation and everything associated with ‘the ivory tower’ in a way that genuinely improves community health.”
SVP and Public & Community lead Letitia Fecher noted that public and community hospital boards are taking a close look at whether and how to partner up with other community hospitals or by joining a larger system.
In other cases, as highlighted by James Cervantes, SVP and Regional Practice lead, systems are creating internal structures such as joint ventures and subsidiaries that allow for innovation and flexibility in how they collaborate.
“Employees are any organization’s biggest ambassadors, and they’re seeing more and more how providers are making cultural investments,” said Partner and Health Services lead Hollie Adams.
Providers are redoubling an already concerted effort to prioritize their people. We’re seeing progress towards more diverse and inclusive environments. There’s greater creativity in how to develop and retain talent. Giving physicians and employees a say in designing solutions to an organization’s unique challenges is one way to both increase innovation and engage the workforce.
All of this bodes well for navigating the ongoing shortage, especially now that we’re seeing what appears to be a new baseline for the role of organized labor in healthcare.
Across the board, our practices are seeing the need to continue addressing the anti-hospital rhetoric and antitrust activity that has taken hold among corners of the media, politics, regulators and healthcare industry itself. In this environment, providers need to be quick to answer the question, “What’s our value proposition?” Cervantes asked, in the voice of an executive leader, “How are we different from the competitor down the road, even if we’re a regional system and they’re an academic center?” Healthcare marketing and communications teams must be involved in developing and then proactively presenting the answers to those questions.
There’s a governance element to this, as well. Provider organizations looking to make patient-focused changes must ensure they have a genuine financial and political commitment to amplify changes and advance things like price transparency. The board and executive team should be aligned on this work.
Regardless of their environment, people still crave interaction. Healthcare leaders and marcomm teams need to use all the tools and technology available to communicate clearly and rapidly, ensuring people know what’s going on – even when what’s going on might be uncomfortable. “We’re in the people business,” said Fecher. “We should be moving faster and communicating that we’re evolving faster.”
Multiple practices saw an uptick in cybersecurity incidences, and it has been a particular focus for our Health Services team. Careful preparation for a potential incident is vital, noted Adams. While a cybersecurity situation is never a good thing, one win our team observed in 2023 was better preparation for and response to incidents. Our team expects the need for this work to continue – the bad actors aren’t going anywhere. Organizations can get through, though, it with close alignment of communications, legal, operations, IT and others.
Our Health Services Practice serves the unique needs of innovative companies, including those backed by PE, focused on advancing healthcare outside the acute-care setting.

Growth strategy. This year we saw significant changes in transaction activity. It’s been much lighter than in years past, which has pivoted growth strategy to be focused more on same store growth than with acquisitive growth. As a result, firms have been encouraging internal engagement and ensuring that their current assets are growing – for example with a focus on patient acquisition – to strengthen existing investments.
That also includes bringing awareness to their brand both externally and internally, and ensuring that how they project themselves externally is reflected in who they are internally. Part of this is connecting with employees through engagement and culture work. Employees are the biggest ambassadors that any organization has and they understand what’s going on.
We saw a significant uptick in cybersecurity incident events, across all of our clients in 2023. The continued push towards greater digital assets and greater digital integration continues to set organizations up for those risks and vulnerabilities and being able to manage effectively through crisis. But, we’ve seen positive results with clients who have gone through data incidents with no scars. This will continue to be a vulnerability in the new year.
Going back to growth and acquisition, in the absence of high deal volume each transaction is even more important. So, we’re seeing attention on recruitment, internal positioning, value protection and in some cases holding on to investments a little longer than a PE firm had planned.
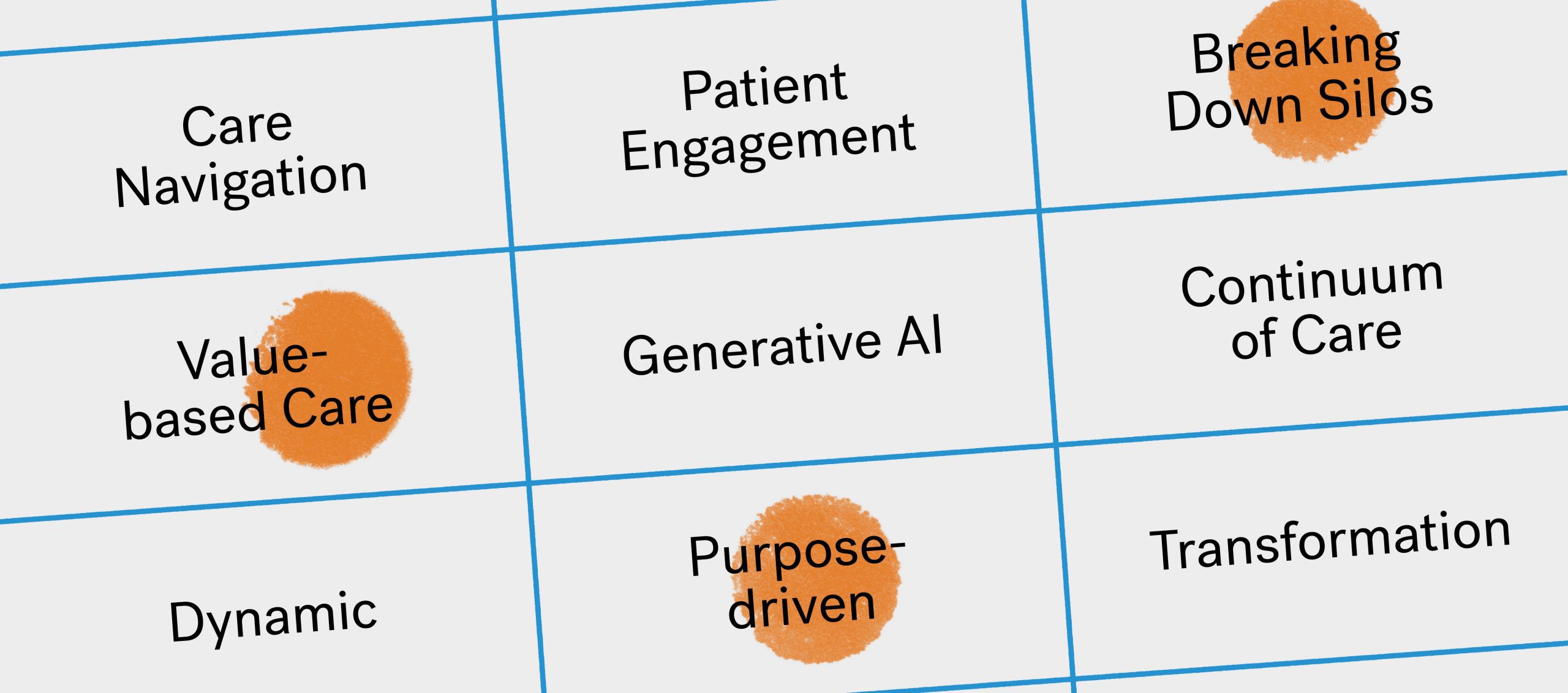
In 2024 we’ll see a heightened focus on value-based care. From a communications perspective, it’ll be important to advance the understanding of value-based care, as well as the financial and reimbursement pressures facing value-based care. Over the past few years, we’ve worked with several value-based care clients on helping them position themselves and articulating their value proposition, who they are and what exactly they do.
It will be interesting in an election year with the heightened scrutiny on providers. The antitrust lens is strong, and there’s a close eye on PE. Health services companies will need to be prepared for that. Each provider should go into 2023 ready to answer the question, “why are we essential to the ecosystem, what data do we have to back it up and what story do we have to explain it.” There can be no gap between how team members and patients/the public perceive these organizations.
Knowing that there are so many challenges, we tend to want to boil the ocean instead of prioritizing issues and creating solutions for them. As a result, one key question would be, “What is the greatest problem we need to solve for.” Then coming up with key priorities around the answer and identifying the top three or so things. If we could do nothing else, what are the top three things we need to address – whether that’s improve access for communities, improve our bottom line, grow a platform or set of services.
It’s identifying the problem we’re solving and who we’re solving it for. One challenge we often run into is that organizations want to see themselves as the central figure in the story. But we need to put things in the proper context – the organization isn’t the hero, it’s the guide. If we can get people into that mindset everything flips and we start seeing the value proposition become clear because, again, we’re focused on the problem we’re solving and for whom. That conversation unlocks everything.
We’re seeing more partnerships and greater alignment between health services and health systems leading to opportunities to increase access in communities and for enhanced growth and profitability. We’ve seen a lot of new activity within the behavioral health space with health services companies partnering with health systems. It’s exciting because there’s investment towards addressing the high demand for behavioral health services.
There’s also the excitement and opportunity around artificial intelligence in healthcare and how providers can integrate AI in various digital platforms. That’s happening in behavioral health, as well. Companies like Synchronous Health are using AI to assess based on an individual’s online activity their risk for behavioral health challenges and then help people recognize those triggers and address them.
This will sound wild, but when we go to the grocery store we can look at a product and see how much it costs. It’s amazing that we have the technology to tell people how much money the need to spend on a service or product upfront.
Seriously, for all the advance we’ve made in healthcare, just that simple aspect of being able to tell the patient how much their care will cost would blow people’s minds. Of course it’s a challenge because of the shape of the healthcare ecosystem where no one entity owns the answer, and there are a lot of variables. But, when we talk about consumer trust and patient trust, we could move mountains by being able to quickly and simply understand what the cost of care is.
Our Public & Community Health Systems practice serves independent and government-owned hospitals, practices and medical centers at the community level.

Employees are engaged now more than ever, allowing providers to rely less on temporary labor. They have a team of core folks who are there for patients, leadership and the community.
Billing and payer negotiations are always front of mind. About half of community hospitals are independent, and many feel they can’t do this alone. Many have realized they need to enter into a partnership, whether it’s a full acquisition or a merger of equals with another community hospital nearby. So, a big challenge has been exploring with leaders and governance what this partnership will look like.
Thinking internally, we’re dealing with many employees who are not reachable in the same way as others. Nurses, for instance, are not in front of a computer all day with access to email communications. So, engagement is an issue. What we learned in the pandemic is: Yes, we can do virtual. But people still crave interaction, even over the screen.
Leaders need to think and act like communicators. That may mean getting out of their offices and purposefully engaging with people – from those working at the bedside to those working from home.
Everything is always changing — it’s communicating the change that’s the problem. This year, health systems and hospitals need to be better at communicating what they’re doing to evolve and be able to meet the needs of the community. They need to be using technology to evolve faster and tell the stories of that evolution.
First, just being in those conversations for comms leaders is important. We counsel our communications leaders that comms can’t drive operational decisions but can be part of the conversation to talk about the decisions the right way.
Then the question to get unstuck is, What are the solutions we’re providing? We’re making this big, operational change, now how are we making that change less of an issue for our patients and employees — how are we communicating it?
It wasn’t exactly unconventional, but it was successful. We had a client very early in the partnership exploration process. They didn’t know what kind of partnership it would be, but they engaged their community to start making a decision. They did listening sessions with employees in the community and narrowed down priorities for those groups, e.g. “These are the 10 things we want to preserve.” They were not only able to use this they searched for a partner, but also down the road, were able to say, “This is what you told us, and we were actually listening. This is going to be a part of it.” Since then, they found a partner, and they still say this initial surveying was the most important part of the entire process.
Our Regional Health Systems practice provides counsel to hospitals serving a geographic region larger than a single city or community.

A commitment to the workforce. In light of all the labor challenges, particularly around recruitment and workforce shortages, regional systems are reinvesting in their nurses, physicians and employees. They are more focused on fostering a culture of belonging and creating environments that are more inclusive. COVID was really difficult for a lot of these health systems. What we saw in 2023 was a concerted effort to prioritize their people in their workforce.
The biggest challenges continue to be those coming out of the pandemic. 2023 was a very challenging year for a lot of health systems – we saw many with declining operating margins. The financial pressure forces hard decisions on how to cut costs and do things differently at the operational level. And so I think we will continue to see that in 2024, though they will be more prepared knowing what 2023 brought.
Communications challenges continue to revolve around how leaders are reaching specific audiences in different employee groups. Organizations communicated very differently in 2023 — I think leaders realized that how they communicated during COVID isn’t sustainable.
One audience that comes to mind is physicians. A lot of these systems have grown their physician base or are working with partners to bring other physicians into their networks, then struggle with how to communicate with them and stay in front of them, keep them informed. That will continue to be a challenge in 2024.
Externally, a need will be to address the continuing anti-hospital rhetoric we’re seeing play out and looking at how health systems are positioning themselves within their communities, within their states and even nationally. There’s also an element of how providers differentiate themselves in their market – they need a very sharp value proposition.
For regional systems where the calendar year coincides with the fiscal year, it’s a turning of the page. We encourage our clients to embrace that moment and start the new year with an eye towards doing things differently than what didn’t work the year before.
The question I’d ask is, what’s the tone that we want to set for 2024 across our organization? The second question is: what will prevent us from getting there? What’s going to stand in our way? What are our barriers from achieving that vision or that tone we want to set?
And then the followup for an executive team is, what are we going to be doing specifically to drive that down through the organization? How are we going to set the tone all the way down to staff on the front line?
We’re seeing a lot of regional health systems smartly partner with non-traditional provider organizations in order to enhance their revenue streams and combat some of the financial challenges they’re continuing to face. So that diversification is part one.
Another example is, I think what some of these regional health systems are doing right now is thinking less about a specific business methodology and more about how they can be flexible and agile in how they operate on a day to day basis. That means empowering all levels of your organization to problem solve; to innovate; to ideate.
Many regional systems are also looking to focus more on delivery of care and offload some of the – to put it bluntly – expenses that are maintained when an organization has a broad portfolio. Things like revenue cycle and supply chain are being outsourced more and more.
I would love to see healthcare providers, and regional systems in particular, be more bold with digital technology and transformation. What if there was a way for patients and consumers to design their own healthcare experience? Or, there was true integration of health information across all your devices, providers and platforms?
I’d also like to see regional systems figure out an effective, cost-efficient way to integrate AI and virtual reality into their care delivery. For example, leveraging AI to provide real-time health updates to patients, help consumers track, monitor and refill prescriptions and or embed it into way-finding when you visit a facility. What’s more, imagine using virtual reality to walk a patient through a process or procedure before it happens so they know what to expect. I think if health systems want to compete with Amazons of the world, they’re going to have to think digital and consumer-first.
Our Academic Health Systems practice provides counsel to academic medical centers and systems – organizations with academic, research and training programs.

We’ve seen positive progress in the number of academic clients who are figuring out both who they’re going to be and how they can best serve their communities. With more academic medical centers and health systems partnering with community health hospitals and health systems, that’s bridged the gap between the ivory tower and community health as they’re looking at different ways of providing care. A great example of this and an area where academic healthcare is uniquely positioned to lead is hospital-at-home. That’s an area where tapping into the innovation and the financial strength of academic healthcare is helping to push patients towards getting care at home when they don’t actually need a hospital.
There are the obvious, industry-wide pressures: Tension with payers is one. Labor is another, it’s been a big story this year. We’ve all been talking about labor for years, and this year the balance really tipped. That’s not going away. Academic health systems have a different set of internal politics when it comes to labor. They have a much more politically diverse constituency in universities with their faculty, so that adds complexity to how they address these issues.
Beyond that, an interesting challenge – or opportunity – is with physician relationships. Particularly as academic systems are acquiring or affiliating with community hospitals. You’re bringing in community docs who may not want to be affiliated with the academic system, and you have academic faculty who want to remain delineated from other physician groups. So an interesting challenge is figuring out how those groups work together and how they’re compensated.
Across all of these areas [above] there’s a significant opportunity for communications-as-strategy. That’s where communications leaders ought to be playing. Given other technological developments that we’ve been talking about over the last year, the time of a communications department being the place that generates newsletters is ending. Thinking about the internal and external political ramifications of all of the ways that academic health systems are growing is probably the highest and best use of communications leaders and communications strategy.
“What are we trying to accomplish? What is the end goal here?” At Jarrard, we talk about “what’s the win?” That’s another way of saying it. Sometimes people get stuck in process or hurdles and if we can work backwards from that, staying focus on the end result we’re striving for in any given endeavor, it’s a useful way to reframe how to get there.
The biggest opportunity for health systems is partnerships with community health providers and systems. There was a big piece in Modern Healthcare recently about how those partnerships will continue to pick up. That’s an interesting combination. It’s getting at finding the best path forward to combine academic capabilities, innovation – all the things that are associated with the ivory tower – with true community health. Providers are figuring out how to develop a shared mission and how to pull the best from each other while leaving some of the excess behind.
It shouldn’t be a weird idea but something we’ve talked a lot about this year is wanting to see healthcare providers get on the front foot as far as what their value proposition is to consumers. Healthcare providers are still far too slow to advocate for themselves in the face of some fairly founded attacks and some unfairly founded attacks from people with a wide range of entrenched interests.
Something like price transparency is a good example. It’s illustrative because hospitals have been attacked on price transparency. They were dragged by regulatory activity into a machine learning world without taking the lessons of what the attacks were based on. And, what they were based on was, “We don’t understand how any of this works, can you please explain it.” Hospitals didn’t explain it enough, so the provider side of the industry needs to think about how to genuinely make changes that are made with the patient in mind, then show a genuine financial and political commitment to amplifying those changes.
Our National Health Systems practice provides counsel to provider organizations with a footprint that covers multiple regions, divisions or communities across the country.

A big win for making healthcare better is how large national health systems have partnered with institutions of higher learning to not only help to solve the long-term issue of workforce shortages, but also help create a healthcare workforce that looks like the community that they serve. A couple examples include the CommonSpirit -Morehouse School of Medicine partnership to what HCA is doing with HBCUs and HSIs across the country and with their new medical school.
The biggest challenge that I helped a national client with this year was a system-wide cyberattack that hit a system of more than 20 hospitals. It brought all of their operations to a screeching halt and they had to go back to operating on paper and caring for patients without any sort of IT infrastructure. Then they had to communicate across every facility about what was up, what was down, and what was happening next.
Across the board we’re seeing large national health systems with big targets on their back. They’re big brands with large footprints across the country, so there’s a lot of interest in preparing for various issues and advocating for either their nonprofit status or for their place in the community.
As we look ahead to an election year, that’s not going to change. Healthcare is going to be a major theme both in the presidential election, as well as state and local elections. Health systems will continue to be asked about their position on a number of hot topics. They really want to be prepared to answer those and to answer them consistently across their footprint.
What I’d love to say is, “What would Dolly do?” Because I love Dolly Parton. But my real answer is that we want to get clients really focused on the single most important thing that they need their people to know, to say, to do. If we can take whatever issue it is and boil it down to a sentence or two, that helps them focus in on what the most important thing is. Then it’s about figuring out the right channel and the right cadence and the right spokesperson. Focusing on that key message about what we’re trying to accomplish tends to break the ice a bit.
It goes back to my earlier answer about large health systems partnering with institutions of higher learning and community organizations to solve for some of the labor shortages that we’ll continue to face for years and likely, decades. I recently spoke with a client that had just released their quarterly earnings. Labor costs were a contributor to less than perfect earnings numbers. We’re not going to be able to fix that until we have more qualified healthcare workers who can jump in and work at a health system and then want to stay through strong retention efforts.
One thing our clients have learned is how to reach frontline workers. They’ve learned this not only from other healthcare organizations but other, disparate organizations where employees aren’t on a computer all day. I was at a conference earlier this year and listened to how brands like UPS and FedEx are reaching their their drivers and warehouse staff. How large convenience store chains were reaching their employees that often only work in pairs and are really far removed from a corporate office. It was fun to hear those examples of how they’re using platforms like FirstUp to reach employees and then to have a discussion with health system clients about how can we implement similar technologies and similar strategies to create systemness. It all goes towards getting people to rally behind an organization’s mission, vision and values.
There are a lot of PHI challenges to replicating in healthcare many of the experiences I enjoy as a consumer. But I would love for someone to come up with a solution that keeps your data safe and secure, but also helps tell you as the patient, what you need and what you should be doing for your health beyond just going to your primary care physician once a year.
I’d love to see a more dynamic, ongoing relationship and experience. Target knows what I want and sends me ideas. Amazon does the same. I wish that I had a healthcare provider that could do that, and I think anything is possible. PHI challenges have certainly slowed progress, but it would have not only a huge impact on those of us who live busy lives, but also those who need more education around how to be healthier, how to make good decisions and when to seek care.
Subscribe to Our Thinking, valuable insights for healthcare execs, communicators and marketers.