We’ve had a few weeks to absorb the news of Amazon’s latest foray into the healthcare space. And we’ve mulled over the words of Neil Lindsay, Amazon’s health services chief, who told the Wall Street Journal on the day of the announcement:
“’We think healthcare is high on the list of experiences that need reinvention,’ said Neil Lindsay, senior vice president of Amazon Health Services. ‘We see lots of opportunity to both improve the quality of the experience and give people back valuable time in their days.’”
Reminds us of an anecdote shared by John Sculley, legendary former CEO of Apple and Pepsi. In a famous story, he recounted how he helped create the two-liter soda bottle, redefining beverage delivery. Seems people wanted more soda at home, but glass bottles were a pain to deal with – expensive, heavy, breakable and hard to deliver. So, Pepsi worked with DuPont to build a light, large plastic bottle. The rest is history.
Sculley drew parallels between his two-liter bottle and healthcare. The current model, he said, is complex, unwieldy, expensive and hard to deliver. It’s ready to be bottled in a different way. In a way that people want and need.
Primary care is ready for its own two-liter bottle. Apparently, Amazon thinks the same.
Now that the initial wow factor of that news has passed, the long-term outlook for the Amazon-One Medical deal and its impact on healthcare in general is hazy. But some hints of change are emerging, including what appears to be an 1849-style gold rush.
David Smith, founder and CEO of healthcare advisory firm Third Horizon Strategies noted that the intensity around this deal feels a bit different. For years, he said, there was “exuberance” that care delivery would be rethought and reworked through disruptive outsiders. And there was activity that created change at the margins. But, generally, no massive disruption. Referencing Haven, Amazon’s previous high-profile healthcare venture when it partnered with Berkshire Hathaway and JP Morgan Chase, Smith said that while it was a highly touted, “It was the first time I saw something of a collective yawn. There was an element of, ‘We’re not buying it, this time.’”
He maintains now that the pendulum has swung back with the One Medical news. Though unconvinced about how truly disruptive it will be in the end, the buzz he’s hearing is that it has “disruptive potential.”(For more on why Smith is a skeptic, see our Q&A with him here.)
Consumer preference continues to grow as a major force for disruption in healthcare.
Amazon wants to be a leader in “dramatically” improving the consumer experience when it comes to healthcare. For years, healthcare insiders have talked about an industry that’s facing disruptive forces and needs to improve. The catalyst? Consumer choice. While others are grappling with how to offer that, Amazon, Walgreens, Walmart and CVS have developed strategies that are deeply informed by their understanding of consumer behavior. Their challenge has been working through the care delivery part. So, this may be the moment when the stars align as a major force for change. One Medical is a consumer play and among the first of its kind from inside healthcare. Their new owners have essentially defined the modern consumer experience.
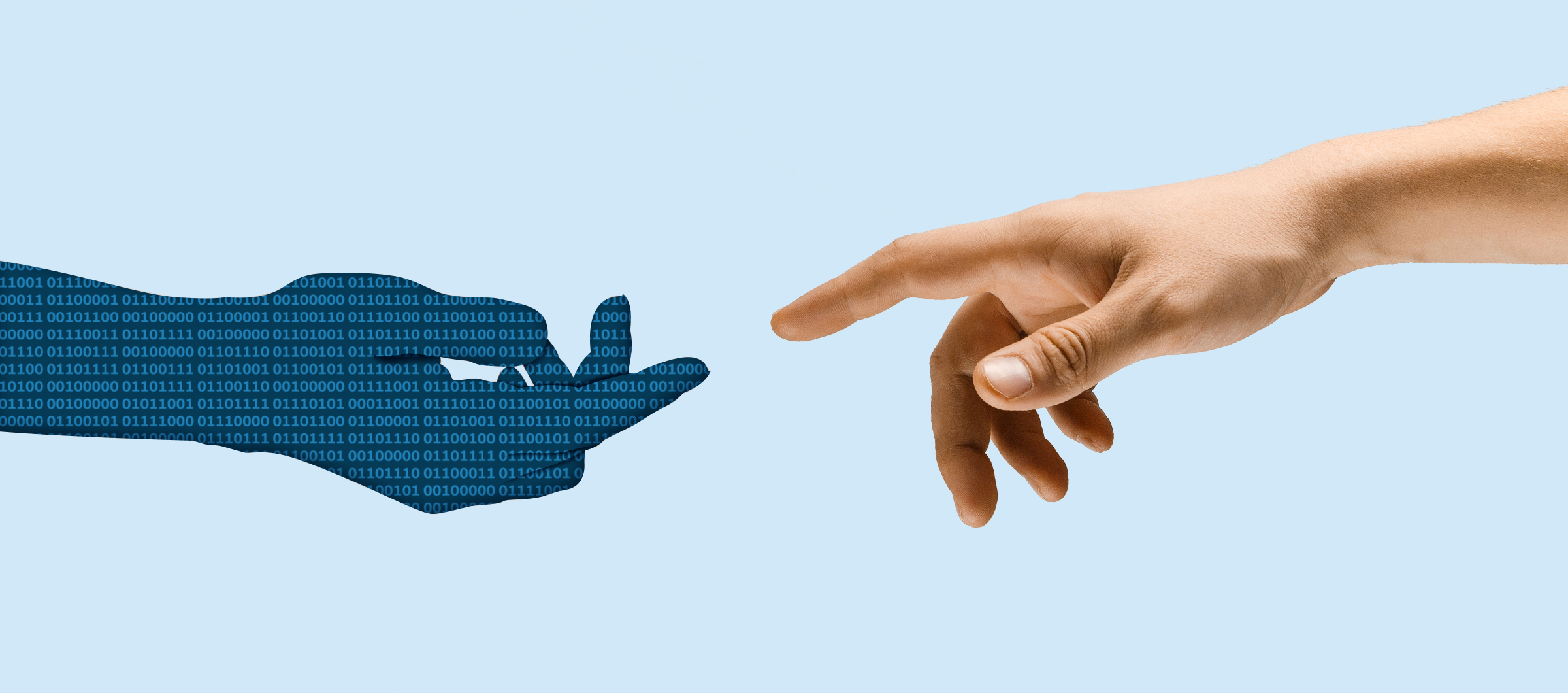
Smith said that Amazon has “an intriguing perspective to delivering care” as a tech business able to amass important information on its users and create a more frictionless, seamless and even integrated experience for patients. “If Amazon can bring that discipline to how a person thinks about their health and how they interact with the healthcare system, that’s something to be excited about,” he observed.
It reinforces the enormous business potential of primary care.
Primary care is valuable and essential. It’s an entry point to the rest of the system and critical for managing health. But primary care has low margins and needs scale to succeed on a business level. That’s hard to do, yet necessary for patients. And it’s attractive for investors who are ready to find that scale. Over the 15 years of its existence, One Medical has taken the time to build a model that appears to work, that people like and that has some traction. Amazon recognizes that steady growth.
Still, there’s a long way to go. “If Amazon/One Medical can activate the demand side and create a bolus in scale, that will make them a power center,” said Smith. “But the pathway will require far more scale than One Medical has today.” Critically, he said, it will also take a lot of trust for people to be comfortable shifting from buying their books and office supplies and baby formula to buying healthcare.
It demonstrates that Amazon isn’t backing down from the challenge of reinventing healthcare.
Depending on your perspective, Amazon and Optum have been either the bully or the hero in pushing transformation on the industry. So far, Amazon’s movement has been limited. It’s been sandboxing ideas, testing opportunities. As our colleagues at The Chartis Group put it,
“The company’s earlier investments and ventures (including PillPack, Halo, Amazon Care, and even Haven) seem to have provided learnings and building blocks.”
This is their biggest healthcare play yet. And it also feels different. It shows that, despite its failed Haven dance party with JP Morgan and Berkshire Hathaway, Amazon isn’t walking away. In one sense that’s a challenge to established players. But it can also give confidence to others, particularly in the health-services realm. It’s a signal that these types of plays are worth risking. We don’t know how this will shake out, but we know the healthcare sector is exposed both in the customer experience and the innovative process. Whatever happens with this marriage will affect both of those things and provide some validation for others.
It strengthens the case for a future in which hospitals are centers for acute care. Period.
As non-traditional players and health-services organizations redefine the consumer experience and build new models of care, there’s obvious pressure on hospitals and health systems. This points to hospitals slowly trending as places where really sick people will go.
Furthermore, it strengthens the emerging blend of virtual and in-person services that’s already re-written the rules for retail. Sri Mani, a director in The Chartis Group’s Private Equity Advisory and Strategy practice, said that this was one of his first thoughts when seeing news of the acquisition. “It begins to signal that a company that is built on virtual provision of services recognizes that not everything can be virtual,” he said. “Some things such as healthcare need a human touch.”
In this deal, he noted the hybrid of virtual and retail needed for primary care today. For traditional providers, it’s finding the appropriate blend by shifting from in-person to virtual, and for Amazon, it’s about shifting in the opposite direction. “They’re going to help us establish what the balance is,” he said.
This blended, hub-and-spoke model of care is becoming a reality. But the spokes aren’t necessarily owned by the hub. This doesn’t have to be unwelcome news. In fact, it might be liberating. Hospitals and health systems can use that to their advantage – taking bigger risks towards projects designed to improve the patient experience. Opening the door to new partnerships. Working with disruptors to create a referral pipeline so that each organization is providing the care it’s best suited to – and in the most efficient, convenient, cost-effective way. Eventually, that benefits everyone, even if the transition is painful. Amazon isn’t backing down, but it also has a long way to go. That leaves the door open to traditional providers and health services companies to do what they do so well while continuing to add a virtual component to care delivery.
It signals the start of the next phase in Big Tech’s healthcare landgrab
In the past year, several big acquisitions, partnerships and explorations have come to light, including a couple since the Amazon news: